
The Drowning Point
Every day, clinicians wade through an ocean of patient data. They drown in it. The average physician now spends two hours on documentation for every hour of direct patient care. This isn't sustainable. The burden crushes morale. It drives burnout. It compromises care.
Behind hospital doors, a silent crisis unfolds as healthcare professionals navigate increasingly complex documentation systems that were meant to improve care but often achieve the opposite. Electronic Health Records (EHRs) have become sophisticated repositories of patient information, yet they've simultaneously transformed into labyrinths that few can efficiently navigate. The promises of digitization—better coordination, fewer errors, data-driven insights—remain frustratingly out of reach for many organizations despite billions invested in infrastructure.
The healthcare industry finds itself at a pivotal inflection point: continue struggling with documentation systems that exhaust practitioners and fragment information, or embrace emerging technologies that can fundamentally transform how we interact with medical information. This isn't merely about efficiency—it's about reclaiming the human element of medicine by liberating clinicians from their keyboards and screens.

The Documentation Avalanche
The statistics tell a sobering story. A 2023 Mayo Clinic study revealed that physicians spend an average of 4.5 hours daily interacting with EHR systems—nearly double the time spent a decade ago. A single hospital admission generates between 60 and 140 pages of documentation. The average patient record contains over 700 data points spread across multiple systems, formats, and structures. Clinicians must process this volume while making critical care decisions.
Documentation requirements have expanded exponentially with regulatory changes, reimbursement requirements, and quality reporting initiatives. The 21st Century Cures Act and subsequent information blocking rules, while designed to improve information sharing, have inadvertently increased the documentation workload. Meanwhile, the Office of the National Coordinator for Health IT reports that the average hospital now maintains connections to more than 15 distinct clinical information systems.
The cost extends beyond time. A 2022 analysis in JAMA Internal Medicine estimated that documentation burdens directly contribute to approximately $90,000 in lost revenue per physician annually through decreased patient throughput. More alarmingly, 54% of physicians reported symptoms of burnout with "excessive documentation requirements" cited as the primary contributor. Patient care suffers—studies show that physicians who spend more time on documentation make more diagnostic errors as cognitive fatigue sets in.

The Agentic AI Revolution
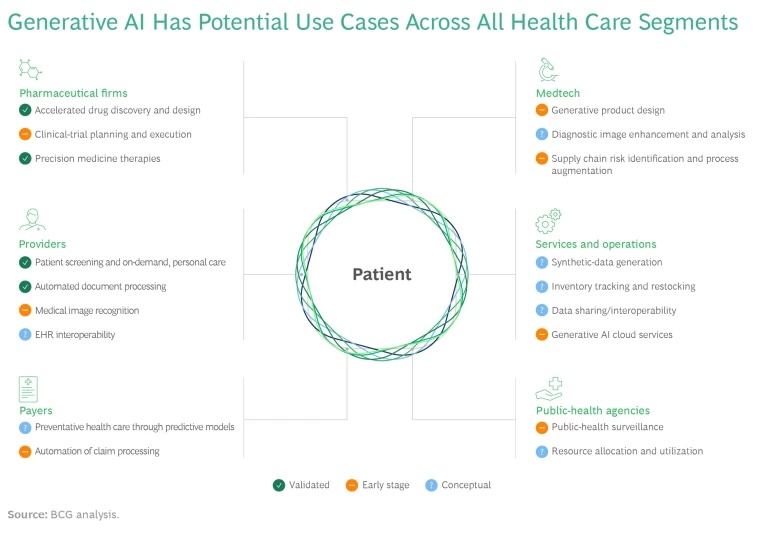
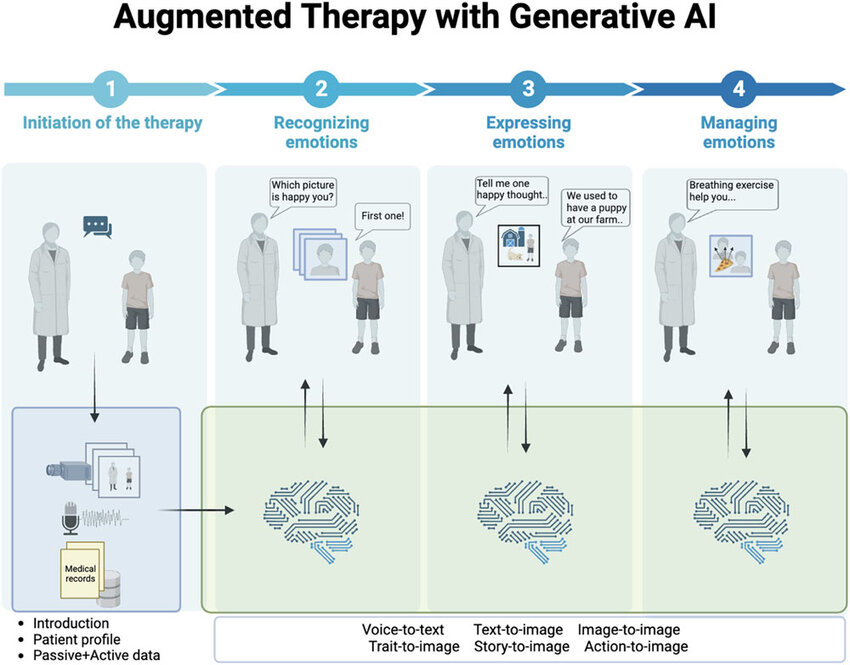
Enter agentic AI—a fundamentally different approach to artificial intelligence that goes beyond simple pattern recognition or predictive analytics. These systems don't just analyze; they act with purpose. They understand contexts. They navigate complex information environments autonomously to complete specific tasks.
Traditional AI examines data and makes predictions. Agentic AI takes the additional step of executing actions within defined parameters to achieve goals. This distinction transforms how AI can interact with medical documentation. Rather than simply flagging abnormal lab values, an agentic system can contextualize that information within the patient's history, recommend appropriate next steps, and even prepare documentation of its reasoning process.
The technical architecture distinguishes agentic systems from their predecessors. They incorporate large language models (LLMs) with domain-specific training, reasoning capabilities that mimic clinical thought processes, and autonomous workflow engines that navigate complex information environments. Most importantly, they learn from feedback through reinforcement learning systems that continuously improve performance through interaction with human experts.
The Medical Record Complexity Challenge
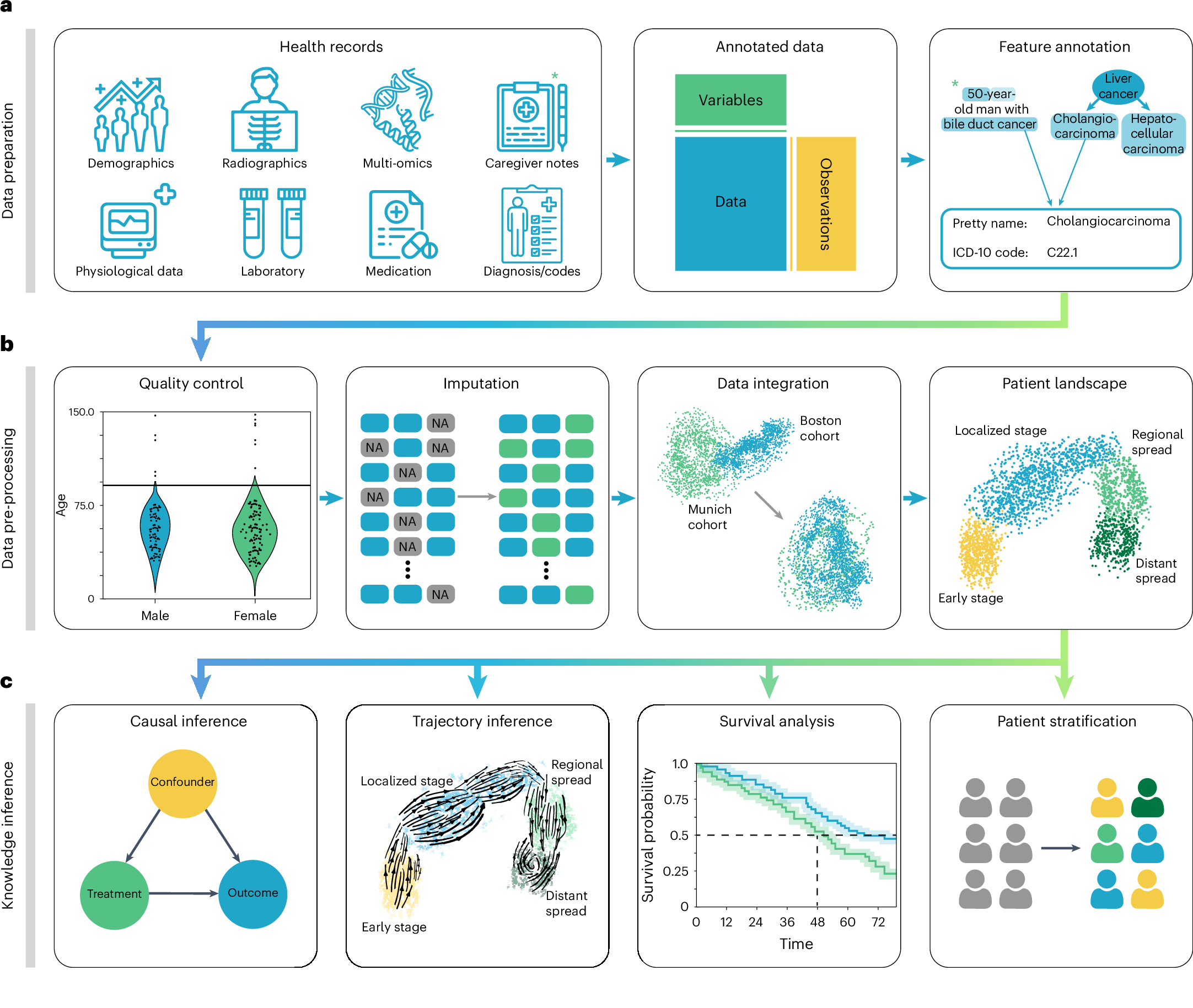
Medical records present unique challenges that have frustrated previous automation attempts. They combine structured data (lab values, medication lists), semi-structured information (templates with free text fields), and entirely unstructured narratives (physician notes, consultation reports). The information varies wildly in length, format, and completeness.
Consider a typical patient hospitalized for pneumonia. Their record might contain admission notes, daily progress reports, nursing documentation, respiratory therapy notes, radiology reports, medication administration records, and discharge summaries. Critical information hides within each document type, often expressed differently depending on the author's training, specialty, and documentation style.
Beyond structural complexity, medical terminology itself presents barriers. A single condition might be referenced by formal diagnostic codes (ICD-10), colloquial terms ("heart attack" vs. "myocardial infarction"), acronyms with multiple meanings (MS could indicate multiple sclerosis, mitral stenosis, or mental status), and implicit references ("the previously noted condition"). Temporal relationships further complicate understanding—distinguishing between historical conditions, active problems, and future considerations requires sophisticated contextual awareness.
How Agentic AI Transforms Documentation Workflows
Agentic AI systems approach medical documentation with capabilities that mirror human cognition while exceeding human processing capacity. The most advanced implementations operate across four dimensions: comprehension, contextualization, action, and adaptation.
In the comprehension phase, agents parse documents regardless of format, extracting meaningful clinical concepts and their relationships. A JAMA Network Open study demonstrated that advanced LLM-based systems achieved 91% accuracy in extracting key clinical elements from unstructured notes—comparable to experienced medical abstractors but operating thousands of times faster.

Contextualization represents the crucial second phase where isolated data points transform into meaningful clinical narratives. The agent evaluates information against patient demographics, medical history, treatment guidelines, and institutional protocols. For example, when reviewing medication lists, the agent automatically flags potential interactions based on the patient's complete profile rather than treating each prescription in isolation.
The action phase distinguishes truly agentic systems from passive analytical tools. Based on comprehension and contextualization, the agent undertakes specific tasks autonomously—summarizing extensive documentation for quick clinical review, preparing draft responses to clinical queries, pre-populating documentation templates with relevant information, or routing specific findings to appropriate specialists.

Real-world Applications Transforming Healthcare
Several pioneering healthcare organizations have implemented agentic AI systems with remarkable results. Boston Medical Center deployed an agentic documentation assistant for their emergency department in 2023, reducing documentation time by 47% while improving compliance with quality measures by 22%. The system doesn't merely transcribe—it actively listens to provider-patient conversations, extracts relevant clinical information, organizes it according to documentation standards, and presents structured drafts for physician review.
At Mayo Clinic, specialists use agentic systems to navigate complex cases requiring review of extensive historical documentation. The system autonomously constructs comprehensive patient timelines from fragmented records, identifying key clinical events, treatment responses, and potential patterns that might otherwise remain hidden in thousands of pages of documentation. Physicians report that this capability has directly contributed to changed treatment plans in approximately 14% of complex cases.
The Veterans Health Administration has implemented perhaps the most ambitious application—an agentic system that continuously monitors documentation across its extensive network, identifying gaps in care documentation that could affect quality measures or reimbursement. Rather than simply flagging issues, the system takes the additional step of drafting appropriate documentation updates for provider review, resulting in a 31% reduction in denied claims related to documentation deficiencies.
Implementation success stories share common elements: phased deployment beginning with limited-scope use cases, rigorous validation against human performance benchmarks, and close collaboration between technical teams and clinical users throughout development and deployment.

Navigating the Regulatory and Privacy Landscape
Healthcare's regulatory complexity presents unique challenges for agentic AI deployment. HIPAA compliance forms only the foundation of a comprehensive governance approach. More specific regulations like the 21st Century Cures Act's information blocking provisions, state-level privacy protections, and professional licensure requirements for documentation all impact implementation.
The Office for Civil Rights (OCR) has begun addressing AI in healthcare directly, issuing guidance that covers agentic systems specifically. Their framework emphasizes accountability—agentic systems must maintain comprehensive audit trails documenting every action taken and decision made. This presents technical challenges but ultimately strengthens trust in these systems.

Privacy protection takes new forms in agentic architectures. Unlike traditional systems with static access controls, advanced agents implement dynamic "privacy by design" approaches. They automatically apply appropriate de-identification techniques based on the specific use case, maintain strict data minimization practices, and implement granular access controls that restrict information flow based on user role and clinical necessity.
Organizations implementing these systems have found success with governance structures that include clinical leadership, privacy officers, legal counsel, and technical experts. Regular third-party audits and feedback mechanisms for patients concerned about AI use in their care form essential components of responsible deployment.

Implementation Realities: Beyond the Technology
Technical capabilities only represent half the implementation equation. Cultural and organizational factors often determine success or failure more than the technology itself. Clinician acceptance remains the most significant hurdle—understandably so, given the high stakes of medical decision-making.
Successful implementations share several approaches to building trust and adoption. Transparency about system limitations proves critical—overselling capabilities inevitably leads to disappointment and rejection. Stanford Health Care's approach exemplifies best practices: they began with a six-month shadow period where the agentic system processed documentation but its outputs remained visible only to the evaluation team. This allowed comparison with human performance without affecting workflows.
Training represents another crucial factor often underestimated in planning. Clinicians need more than technical instruction; they require a conceptual understanding of how the system works, where its limitations lie, and how to effectively collaborate with it. Organizations that invest in comprehensive education—typically 4-6 hours of initial training followed by regular updates—report significantly higher adoption rates.
The financial model must also align with organizational realities. The most successful implementations tie funding directly to measurable outcomes: reduced documentation time, improved coding accuracy, decreased denial rates, or enhanced quality scores. This outcomes-based approach ensures continued executive support beyond initial implementation enthusiasm.
The Near Horizon: What's Next for Agentic Systems
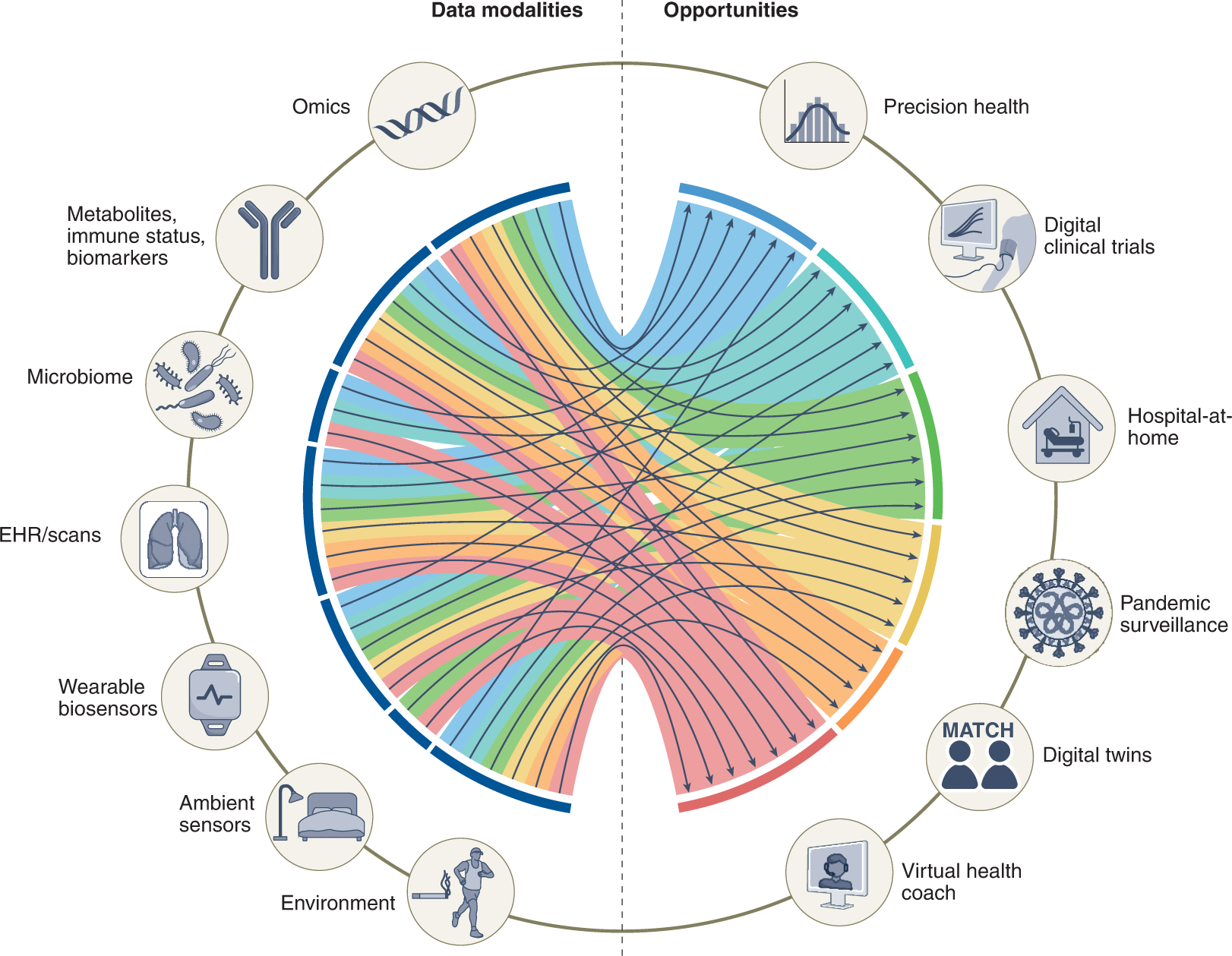
The next generation of agentic documentation systems is already emerging in research settings. Three capabilities appear particularly transformative: multimodal understanding, collaborative reasoning, and proactive insight generation.
Multimodal understanding enables agents to process not just text but images, audio, and video simultaneously. Applied to healthcare documentation, this means systems can interpret medical imaging alongside clinical notes, incorporate bedside conversations, and even analyze patient movement patterns from video for functional assessments. Early research at University of California San Francisco demonstrates systems that can review dermatology images alongside clinical descriptions to generate more comprehensive documentation than either modality alone could support.
Collaborative reasoning represents a shift from AI as tool to AI as teammate. Next-generation systems explicitly model their own uncertainty and proactively request clarification when needed. They explain their reasoning processes transparently, allowing clinicians to understand not just what conclusion the system reached but how it arrived there. This capability significantly enhances trust while improving system performance through continuous refinement.
Perhaps most exciting is proactive insight generation—the ability to identify patterns and opportunities that might otherwise remain hidden in complex documentation. These systems don't merely respond to queries but actively surface relevant insights based on their understanding of clinical priorities. A system reviewing documentation might autonomously flag that a patient meets criteria for a clinical trial, qualifies for additional services, or shows early warning signs that warrant preventive intervention.
The Human-AI Partnership
The most powerful vision for agentic AI in healthcare documentation isn't technological but human-centered. The goal isn't replacing clinical judgment but amplifying it—creating systems that handle routine information processing so human experts can focus their cognitive resources on complex decision-making, relationship building, and compassionate care.
This vision requires reconceptualizing documentation from administrative burden to clinical asset. When documentation systems capture the right information at the right time and present it effectively, they transform from bureaucratic requirements to valuable clinical tools. The difference lies not just in what information exists but in how accessible and actionable it becomes.
The path forward requires balanced perspective. Technological enthusiasm must be tempered with rigorous evaluation. The economic pressures driving adoption must be balanced with ethical considerations about appropriate use. Most importantly, the design process must center clinical needs rather than technical capabilities—creating systems that adapt to healthcare workflows rather than forcing healthcare to adapt to technological limitations.
A Call to Thoughtful Action
Healthcare organizations stand at a critical decision point. The documentation burden has reached unsustainable levels, yet powerful new tools offer realistic paths to improvement. Moving forward effectively requires balanced assessment and strategic implementation.
The first step involves honest evaluation of current documentation processes. Before implementing new technology, organizations should quantify existing challenges: documentation time, error rates, clinician satisfaction, and impact on patient care. This baseline establishes both the case for change and metrics for measuring success.
Implementation should follow a measured approach—beginning with focused use cases that offer clear value while limiting risk. Radiology report generation, pre-visit documentation preparation, and discharge summary drafting have proven particularly effective as initial applications. Each provides tangible workflow improvement while allowing clinicians to maintain appropriate oversight.
Throughout implementation, continuous evaluation against both technical and human measures remains essential. Technical metrics like accuracy and processing speed matter, but equally important are human factors: Do clinicians trust the system? Does it reduce their cognitive load? Does it enable more meaningful patient interactions?
The transformative potential of agentic AI in healthcare documentation is clear, but realizing that potential requires more than technology deployment. It demands thoughtful integration into clinical workflows, appropriate governance frameworks, and commitment to measuring outcomes that matter. When implemented with this balanced approach, these systems offer something increasingly rare in healthcare technology: tools that simultaneously improve efficiency, enhance care quality, and reduce clinician burden. The documentation challenge has found its match in agentic AI—not as a replacement for human expertise but as its most powerful ally.
1. What exactly is "agentic AI" and how does it differ from traditional AI systems in healthcare?
Agentic AI systems go beyond analysis and prediction to take autonomous actions within defined parameters. Unlike traditional AI that might flag abnormal lab values, agentic systems can contextualize findings within patient history, recommend next steps, prepare documentation, and learn from feedback. They combine large language models with clinical reasoning capabilities and autonomous workflow engines that navigate complex information environments independently. The key difference is their ability to perform sequences of actions to accomplish goals rather than simply providing information.
2. What's the typical ROI timeline for implementing agentic AI documentation systems?
Most healthcare organizations see initial ROI within 9-12 months of full deployment. Early wins typically come from reduced documentation time (30-50% reduction for most clinicians) and improved coding accuracy leading to appropriate reimbursement. Boston Medical Center recouped their investment in just 7 months through a combination of improved clinician productivity and a 22% reduction in denied claims. Longer-term ROI continues to grow as systems learn from your specific environment and expand to additional use cases. Organizations typically see 3:1 to 5:1 return after 24 months of operation.
3. How do we address physician concerns about accuracy and liability when implementing these systems?
Transparency and governance are crucial. Establish a clinical oversight committee that reviews system performance regularly. Implement a "human-in-the-loop" approach where clinicians maintain final approval authority over all documentation. Create clear accountability frameworks that specify who holds responsibility for content accuracy. Early implementations should include a validation period where outputs are compared with human performance before affecting actual documentation. Most importantly, frame the technology as an assistant rather than a replacement—physicians who understand they maintain control show dramatically higher adoption rates.
4. What infrastructure requirements should we anticipate for deploying advanced agentic AI systems?
Most enterprise healthcare organizations already have the core infrastructure needed. You'll require secure API connections to your EHR systems, sufficient processing capacity (either on-premises or cloud-based), and appropriate data governance frameworks. The most successful implementations leverage hybrid architectures where sensitive data processing occurs within your security perimeter while more computationally intensive tasks use secured cloud resources. Network capacity is rarely a bottleneck as modern systems are designed for efficient data exchange. Your existing disaster recovery and business continuity systems should extend to cover these new capabilities.
5. How do privacy regulations like HIPAA impact the implementation of agentic AI for documentation?
HIPAA actually provides a workable framework for agentic AI implementation when properly applied. Your implementation must incorporate comprehensive audit trails documenting all system actions, appropriate access controls based on the minimum necessary standard, and secure transmission protocols. The Office for Civil Rights has clarified that agentic systems may be considered business associates and should be covered under appropriate BAAs. Some organizations implement additional safeguards like differential privacy techniques that mathematically guarantee patient confidentiality while allowing systems to learn from aggregate data. Your existing HIPAA compliance framework can extend to these systems with thoughtful adaptation.
6. What are the top implementation pitfalls we should avoid?
The most common failure points are insufficient clinical involvement during design, inadequate training programs, poor integration with existing workflows, and overpromising capabilities. Successful implementations incorporate clinical leaders from day one, invest in comprehensive training (4-6 hours initially plus regular updates), carefully map and enhance existing workflows rather than disrupting them, and maintain transparent communication about both capabilities and limitations. Additionally, starting with overly complex use cases often leads to disappointment—begin with focused applications where success criteria are clear and measurable.
7. How can we measure success beyond simple efficiency metrics?
The most valuable metrics combine operational, clinical, and human factors. Beyond documentation time reduction, measure changes in denied claims, coding accuracy, and compliance with quality measures. Clinically, track time spent with patients, satisfaction scores, and potential quality improvements like reduced readmissions or more comprehensive preventive care. For human factors, regularly assess clinician burnout scores, technology satisfaction, and retention rates. The organizations seeing greatest value implement balanced scorecards that track all three dimensions rather than focusing solely on efficiency gains.
8. How do agentic AI systems handle the variation in documentation styles between different specialties and institutions?
Modern agentic systems employ adaptive learning approaches that recognize and accommodate specialty-specific and institutional documentation patterns. Initial deployment includes a calibration phase where the system analyzes existing documentation to identify specialty-specific terminology, organizational preferences, and individual clinician styles. The system continues refining its understanding through feedback loops where clinician edits teach it to better align with expectations. This adaptability means the same underlying technology can effectively serve different specialists and accommodate the unique documentation culture of your organization without requiring extensive customization.
9. What security considerations should our IT team prepare for when implementing these systems?
Beyond standard healthcare security protocols, agentic systems require attention to prompt injection vulnerabilities, model poisoning risks, and comprehensive activity monitoring. Your security framework should include adversarial testing to identify potential manipulation points, segmentation that limits system access to necessary data only, and continuous monitoring for unusual patterns of system behavior. Leading implementations incorporate "explainability modules" that make system decision processes transparent for security review. Partner with vendors who maintain SOC 2 compliance and offer regular security updates as new vulnerability classes are discovered.
10. How will these systems evolve over the next 3-5 years, and how should we plan for future capabilities?
The technology roadmap points toward three major evolutions: multimodal integration (incorporating images, audio, and structured data simultaneously), collaborative reasoning (systems that explain their thinking and appropriately express uncertainty), and ambient documentation (capturing clinical encounters naturally without explicit dictation). Organizations should implement with flexible architectures that can incorporate these advances without complete replacement. Consider contractual arrangements that include technology refreshes and capability expansions. Most importantly, develop internal expertise that can evaluate new capabilities as they emerge rather than relying entirely on vendor guidance for upgrade decisions.

Rasheed Rabata
Is a solution and ROI-driven CTO, consultant, and system integrator with experience in deploying data integrations, Data Hubs, Master Data Management, Data Quality, and Data Warehousing solutions. He has a passion for solving complex data problems. His career experience showcases his drive to deliver software and timely solutions for business needs.




